The Collaborative Relationship
Prosthetist and Patients Co-Create
I am a prosthetist at Hanger Clinic working in multiple offices across Massachusetts. As a prosthetist, I measure, design, fit, and help in maintaining prosthetic devices for my patients.
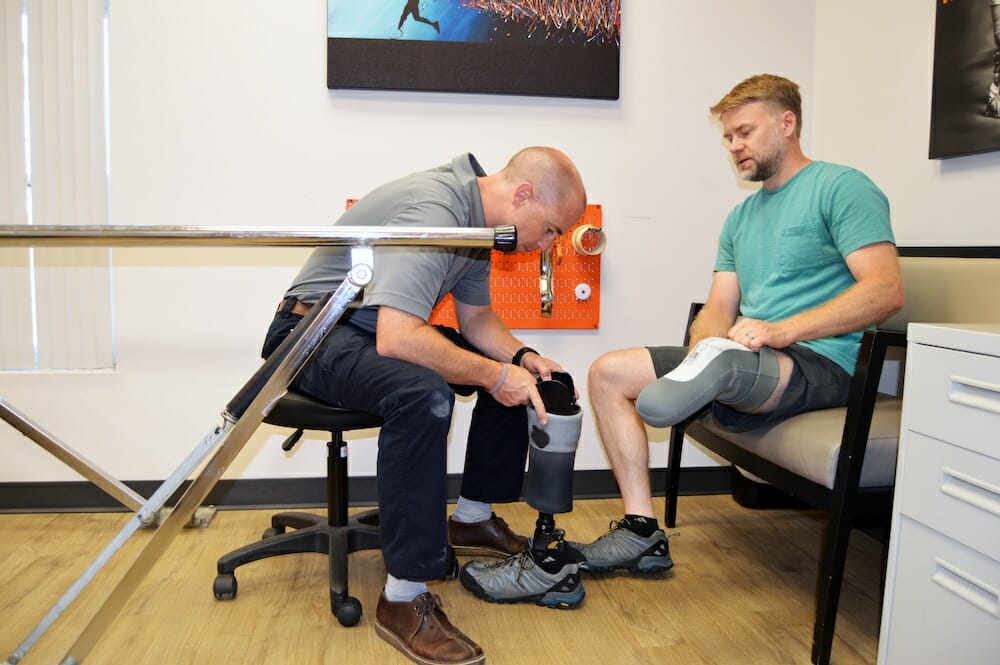
Prosthetist Brian Heckathorn and Steve Woolfenden discuss the fit and feel of Steve’s most recent prosthesis.
By Brian Heckathorn, Area Clinic Manager, CPO, Hanger Clinic; edited by Amanda Hawkins & Grace Mennell
Prosthetists work in various settings including patient care clinics, hospitals, rehabilitation facilities, and in product design and development. I have had the unique opportunity to work closely with individual patients for numerous years as well as innovate and advance prosthetic socket design and development.
Prosthetics and Orthotics
I entered the field of prosthetics during my undergraduate pre-med education at Albion College. I was gaining clinical experience working as a student athletic trainer and had the opportunity to shadow at an Orthotic and Prosthetic company in Jackson, Michigan. What started as a brief job-shadowing experience turned into a semester-long externship, where I fell in love with the mix of challenges, creativity, and the impact prosthetic care has on patients.
At Hanger Clinic we specialize in prosthetic and orthotic products, with an emphasis on patient care, collaboration, outcomes, and innovation. Hanger was started over 150 years ago by a Civil War-era amputee named James Edward Hanger. Since then the company has grown exponentially, with approximately 800 clinic locations nationwide — our organization is a leading provider of orthotic and prosthetic patient care services and solutions.
Our area of practice enables us to be creative, work with our hands, and spend meaningful time problem solving with the goal of improving the functional outcome, and hopefully quality of life, of our patients. With the diversity of required skill sets, we’re seeing people enter the field from wide-ranging backgrounds including healthcare, engineering, technical vocations, art, and design. A deep focus and commitment to patient care defines the practice at Hanger Clinic. We provide care to 1 million patients annually. Going beyond timely and reliable care, Hanger provides access to the innovative collaborations of almost 1,300 clinicians as well as an extensive education and peer support program called AMPOWER.
Advancements in technology are revo- lutionizing our clinical practice. The current curriculum for the Masters-level education required of clinicians almost always includes courses on new technologies ranging from 3D digital scanning, computer-aided design, computer-aided manufacturing, 3D printing, microprocessors, and advanced neural inputs. This knowledge elevates our profession and allows us to more closely partner with researchers, designers, surgical teams, manufacturing, and supply chain partners.

The Hanger Clinic Experience
When a patient first visits one of our prosthetists, our priority is to learn from them, establish their comfort level, explain the overall process, and develop a plan. We want their experience to be different than any other healthcare encounter. From initial greeting throughout all levels of care we strive to make our patients feel welcome, never rushed, and as comfortable as possible. This type of environment fosters open dialogue between the prosthetist, patient, and family. The comfortable environment allows the patients to feel like their every question and request matters. Our dialogue and trust building is critical to make sure that our design matches their needs.
Once the patient’s initial questions have been answered, we conduct a mix of formal and informal evaluations, which help patients with goal-setting and prosthetists with the prosthetic design. Patients typically discuss their short and long-term goals that generally flow from basic daily functional needs to detailing their work and recreational goals. It is always helpful to have a realistic picture of what their functional status was prior to amputation, what is non- negotiable, and then what their true desires are for the device. We also do strength testing, range-of-motion testing, limb inspection, measurements, 3D scanning or plaster casting, and we discuss overall design.

The Design Process
In preliminary appointments and meetings we decide the proper socket design and suspension technique. The socket is the part of the prosthetic device that connects directly with the residual limb. And suspension techniques work to keep the device attached to the wearer while the prosthesis contends with forces of everyday use — for example, some devices create a vacuum seal between the residual limb and the socket for a strong interface and connection. Sockets are custom designed for each individual and need to account for the continued healing process. We discuss the pros and cons of each design and make a team decision.
Once the primary incision has healed, clinicians provide light compression to the residual limb via an elastic sock, called a shrinker, made to control swelling, promote healing, and influence the initial shape of the residual limb. After about two to three weeks following the removal of sutures, we 3D scan the patient’s residual limb — the resulting 3D data helps us form the custom socket. At facilities with in-house fabricators, like Hanger Clinic, skilled technicians use the 3D data to carve the shape into dense foam using a computer-controlled mill. That form serves as the mold for a plastic sheet that is heated — and drawn over the mold — to take the shape of the custom socket.
When we have the socket and build a preliminary design for the overall device in our shop, we perform a diagnostic fitting at the clinic to confirm the fit, assess comfort level, and fine-tune the alignment of the prosthetic limb with the residual limb. Finally, a few days after the diagnostic fitting, the final prosthesis is complete — the patient can take it home and begin rehabilitation. All told, assuming no additional complications, an amputee that is otherwise healthy could expect to be fitted with a prosthesis within three months.

Hanger Clinic’s design studio features traditional handcrafted tools, as well as the newest technology.
Working with Survivors
On April 15, 2013, two explosions near the Boston Marathon finish line killed three people and injured hundreds, 16 of whom lost limbs.
Adrianne Haslet and Steve Woolfenden are both survivors of the Boston Marathon bombing — I am their prosthetist. In each of their individual experiences with surgery, healing, and using a prosthetic device for the first time, they experienced immense shifts in their lives as they learned to navigate a new reality. Since then, Adrianne and Steve, with the help of Hanger Clinic, have accomplished various goals in everyday life, athletics, and overall recovery.
During initial meetings with Adrianne and Steve, we communicated the importance of an early focus on the initial surgical healing and provided them both with stories and imagery to help them envision their ability to return to their lifestyles. Adrianne and Steve had well-defined sets of expectations for work and recreation. Adrianne had specific mobility- goals in mind that would allow her to dance again, and she set a new goal to run the Boston Marathon. Steve expressed an interest in skiing with his son, which led to us fitting him with specifically designed prosthetics that allow him the necessary motion and structure to hit the slopes again.
Adrianne Haslet

“In the days following the attack, I told the world I would run the Boston Marathon, even though I was not a runner. When asked how, I said, ‘There was once a time in my life where I was not a ballroom dancer. Now I am. I am not a runner now, but I can be. And I will be.’”
Adrianne Haslet
Adrianne is the epitome of a determined, motivated person, and from the beginning of her limb loss journey, she was committed to getting back her mobility and working towards her goals of running and dancing. As with many people who have limb loss or limb difference, the process of fitting Adrianne with a prosthetic device that would allow her to reach her goals involved a lot of conversations and open lines of communication. Adrianne is great at providing feedback on how her socket is fitting and feeling, and by incorporating that feedback into her custom-designed prosthetic legs, we’ve been able to help her reach her mobility goals.
She now uses both an everyday leg with an adjustable heel portion, as well as the Fillauer AllPro running foot. As she began training for the Boston Marathon, we worked together to find a blade that allowed her the most motion and didn’t hold her back. Her stride was greatly impacted by the length of the running blade and once she began using the Fillauer AllPro, she felt more comfortable and able to push herself harder. Adrianne continues to dance and run the Boston Marathon with her team, The Heartbreakers.

Steve Woolfenden

“One of the first challenges I
encountered in prosthetics, was a feeling of sadness and depression, as it really emphasized how permanent this situation was.”Steve Woolfenden
When I first met Steve at Boston Medical Center, we clicked immediately. We are both originally from Michigan, we are both athletes, both fathers, and we are close to the same age. During this first visit, it was important for us to let Steve know that there were people available to help him through the process of picking and adjusting to a prosthetic device when and if he was ready.
With Steve, we started off with the question, “what will this prosthetic be used for?” Because Steve has an active lifestyle, I used a scanning system to generate a digital representation of his residual limb in order to design a proper socket. Steve has the option to add graphics that are laminated into the socket. For example, on his water leg, we wrapped the socket with fabric that has a brook trout print. Overtime, changes can occur to the residual limb that affect the overall fit. Steve’s limb has fluctuated over time, at times causing some discomfort for him, which has been solved with adjustments to his prosthetic socket.
I see Steve about every three months. We sometimes just text or call to check in or if smaller, more minor things come up. Steve is a brilliant scientist — he is good at figuring stuff out on his own; in fact, he taught me about repairing sleeves for sockets with the type of silicone typically used to make gaskets. He is also exceptionally good at taking care of his prosthetic devices which helps maintain their function over time.
Lasting Impact
With all patients, we ask if we can check in regularly to make sure their device is meeting their expectations and so we can answer any questions they may have. We also remind them about our commitment to helping them achieve their goals long-term.
Since 2013, Adrianne has gone on to dance again, run the Boston Marathon multiple times, and establish her own foundation for amputees and prosthetic device users. Steve has rediscovered his love of running, biking, and skiing, which he shares with his son. Both Adrianne and Steve continue to work and refine how they use their prosthetic devices. It is an ongoing process of adjustment and growth.
One of Hanger’s core values is measuring and understanding outcomes of care. Along with carefully validated clinical practice guidelines and outcome studies, the lasting impact of Hanger Clinic’s work is visible in the stories of people like Adrianne and Steve.
It has been the honor of my life to be involved in so many amazing people’s life stories. As prosthetists, we are invested in improving the quality of our patients’ lives, therefore a strong bond is developed between patient and prosthetist. You feel the same sense of honor and pride in their evolving accomplishments that you would of brothers, sisters, mothers, fathers, and children. This lasting relationship is just like family.

