Community as Medicine
Re-Designing Healthcare
I’m Dr. Elizabeth Markle. I’m a psychologist, an innovator and entrepreneur in the fields of human health and well-being, a scholar of Intentional Community (literally, community shaped by design), and Co-Founder of Open Source Wellness.

Open Source Wellness participants enjoy a meal and small group coaching. Image courtesy of Open Source Wellness.
By Dr. Elizabeth Markle, Co-Founder of Open Source Wellness
Behavioral Prescriptions
My co-founder at Open Source Wellness, Dr. Benjamin Emmert-Aronson, and I have worked and trained in many different healthcare delivery systems: tiny clinics, federally qualified health centers, massive hospital systems, and the Veterans Administration. Our jobs were to provide mental and behavioral health support to patients, and consultation to doctors struggling with the behavioral aspects of their patients’ care—in clinics, hospitals, and even emergency departments. It was wild, wonderful, and profoundly challenging work!
During this time, we started keeping track of what we now call “Behavioral Prescriptions.” Back then, we just called them, “things that doctors tell their patients to do.” And here’s what we found: no matter the patient’s diagnoses—diabetes, hypertension, depression, anxiety, heart disease, etc.— and no matter the provider’s professional identity, (primary care doctor, specialist, therapist, case manager, etc.), 80 percent of patients were receiving the same four behavioral prescriptions: exercise more, eat better, reduce your stress, get some social support.
These big four behaviors and practices underlie human health and well-being broadly, and they are appropriate “prescriptions.” But here’s the part that made us apoplectic: the doctor would deliver these instructions, and then say something like, “Good luck with that! Take care now!”
Our patients, alone in a tiny sterile room, intimidated and disoriented next to their fast talking, rushed, and authoritative doctor, would look down and meekly say, “Yes, ok, I know, I should, I will, ok…” and that would be the end of the visit. Until the next time we saw that same patient, often in the emergency room, for a predictable worsening of their chronic condition, and the conversation would repeat.
Healthcare providers are asked, and heroically trying, to meet unmeetable needs: to generate and deliver enough care, resources, support, and even love for patients and communities. They are doing so in tightly timed individual visits, in resource-strapped clinics, with ever growing responsibilities and ever-tightening constraints. Shrouded in veils of confidentiality, privacy, and even shame, rapid one-on-one visits don’t necessarily build resiliency, community strength, or capacity to generate health and well-being for our patients. Instead, they can further segregate our healthcare from our daily lives and communities.
Over time, as we watched this choreographed vignette play out, my conversations with Ben started to take on the tone of weary disbelief, and ultimately disgust. I remember saying to him, “Can you imagine prescribing insulin, and saying ‘Good luck finding that! I’m sure you’ll figure it out?’ Of course not. We say, ‘Your medication will be ready for you in an hour at the pharmacy nearest you, paid for by your insurance, and a pharmacist will make sure that you actually know how to take it!'”
Unlike our extraordinary infrastructure for delivering on prescriptions for medication, our nation has no delivery system for Behavioral Prescriptions—the simple, universal practices and experiences that underlie health and well-being. Instead, outcomes divide along lines of wealth and privilege. Patients with privilege (financial and sociocultural) shop at Whole Foods, hire personal trainers and therapists –and those without experience predictable and painful entrenching of chronic physical and psychological conditions.
Healthcare is miserable. Its recipients are isolated and fearful, and its providers are exhausted and demoralized. And it doesn’t have to be like this.
Another Way
We imagined this alternative: A doctor informs a patient that she has diabetes. Instead of saying, “Eat better, exercise more, try meditating, here’s a handout. I’ll see you in six months!” the clinician says, “I’ve written you a prescription, but it’s not for medication. It’s for participation in a community dedicated to well-being. They cook healthy food, do fun physical movement, practice stress-reduction, and support each other in making and meeting the goals that matter most to them. Once you’ve completed your four-month initial dose, which is fully covered by your insurance, they will help you connect with other graduates in your neighborhood who get together to practice, and your whole family is always welcome to join you.”
Ben and I set out to transform the standard of clinical care by creating Open Source Wellness (OSW), so that every Behavioral Prescription would be backed by a Behavioral Pharmacy, a comprehensive delivery system for human health and thriving across each of the four behavioral prescriptions: MOVE (physical activity), NOURISH (healthy meals), CONNECT (social support), and BE (stress reduction).
Open Source Wellness is a nonprofit initiative supporting people and communities in living healthy and happy lives by leveraging “Community As Medicine” in collaboration with healthcare providers and insurers.
When we started, we had a few core design commitments. Open Source Wellness would be:
Experiential: Rather than telling people what they should be doing, via a lecture, a class, handouts, or even a fancy app, we actually DO the practices together, in community. The experience, not the information, is the medicine.
Transdiagnostic: Rather than having “Depression group” and “Diabetes group” and “Hypertension group,” we have Transdiagnostic groups. These groups are diagnostically and demographically diverse groups of participants and coaches who practice together, working with the human challenges of health and well-being, focused on the same universal practices of Move, Nourish, Connect, and Be.
Powered by Connection: Rather than expensive licensed medical professionals, who are typically trained to dispense information from the perspective of an objective expert, OSW is facilitated by culturally relevant health coaches and peer leaders, who engage with warmth, vitality, vulnerability, and humanity.
Democratized: Rather than replicating the boutique wellness industry, OSW was designed to be affordable and accessible to those who need it most, via mainstream healthcare.

Physical activity at Open Source Wellness is designed to be playful, social, and expressive, leaving participants feeling connected and invigorated.
The Patient Experience
As soon as a provider prescribes participation in OSW, the patient gets a phone call from a OSW coach. This is not a quick scheduling or administrative call: this is a spacious, friendly, relationship-building conversation, in which the coach and patient explore the challenges the patient is facing, what they most value in their health and in their lives, and how OSW might be of support. Because of this initial relationship, participants are ready and eager to join their weekly OSW group. And although there is tremendous variation across OSW groups, according to population demographics, location, language, and culture, the basic structure of every OSW session is the same. While in the past these groups ran both in-person and virtually, because of COVID-19 we now run all groups virtually, and provide extensive support to participants who need orientation to videoconferencing.
We start each weekly session with a warm, friendly welcome, very intentionally cultivating a context that feels more like a community block party than a medical group! The group of 20 to 30 participants and three to five coaches begin together with an icebreaker, followed by 20 minutes of fun physical activity. This “exercise” is playful, interactive, and designed to give participants the lived experience and visceral memory of physical activity being fun, enjoyable, and socially rewarding. We then transition to five minutes of stress reduction or mindfulness practice. We share and facilitate practices from no particular tradition and with no dogma, just basic practices for transitioning from high activity, external focus to quiet, inner focus, and stillness. Next is the SPARK, a highly experiential/interactive lesson on a topic related to one of our four pillars (Move, Nourish, Connect, Be), such as eating well on a budget, setting boundaries in interpersonal relationships, or structuring daily routines during a pandemic.
At this point, the large group breaks into small groups which consist of six participants, one OSW coach, and one peer leader. This small group spends about 45 minutes in conversation. It’s not psychotherapy, but it is highly therapeutic, as these intimate groups share about their health and about their lives: their families, their dreams, their aspirations, their traumas, the challenges of their worlds.
Every OSW group ends in a similar way: the large group reconvenes for expressions of gratitude, sharing of offers and requests (in which participants ask for and offer support in the form of accountability or resources), and lastly declarations, in which participants commit aloud to a practice or task they will accomplish during the week in support of their health and well-being.
Frequently, these self-prescriptions are overtly related to health: “I’m going to walk three times this week,” or, “I’m going to cook greens tomorrow night,” or, “I’m going to reach out to a friend that I’ve lost touch with.” But interestingly, we also hear declarations like, “I’m going to tackle my credit card statements this week,” and, “I’m going to floss my teeth every night this week!” While at first we were perplexed, noting that financial health and dental health appear nowhere in our curriculum, we’ve come to understand that when participants start to get traction in the program, experiencing success making and meeting goals, they are naturally moved to take on other meaningful realms of their lives. They develop self-efficacy, confidence, a commitment to their own integrity about doing what they say they will do, and that translates broadly to creating quality of life.
In between weekly sessions, participants are on group text threads with their peers and their coach, and are giving and receiving support and accountability throughout the week. If a patient makes a commitment to exercising every day, the next day her group members will be reaching out and saying, “How are you doing with your exercise today? Any support you need? Send us a photo!” It’s an immensely high-dose, high-touch, socially-supportive intervention that kickstarts proactive, generative, empowered self-care and life-care.
Ultimately, this is what we are committed to. If someone’s blood pressure drops, or their blood sugar comes down, that’s fantastic! If we are able to jumpstart a life, to help someone move from demoralization, passivity, a stance of helplessness and disempowerment toward an active, empowered, positive reward-seeking approach to life, the implications are immense.

Meals at Open Source Wellness are plant-based, and designed to give participants the experience that whole foods can be delicious!
Outcomes
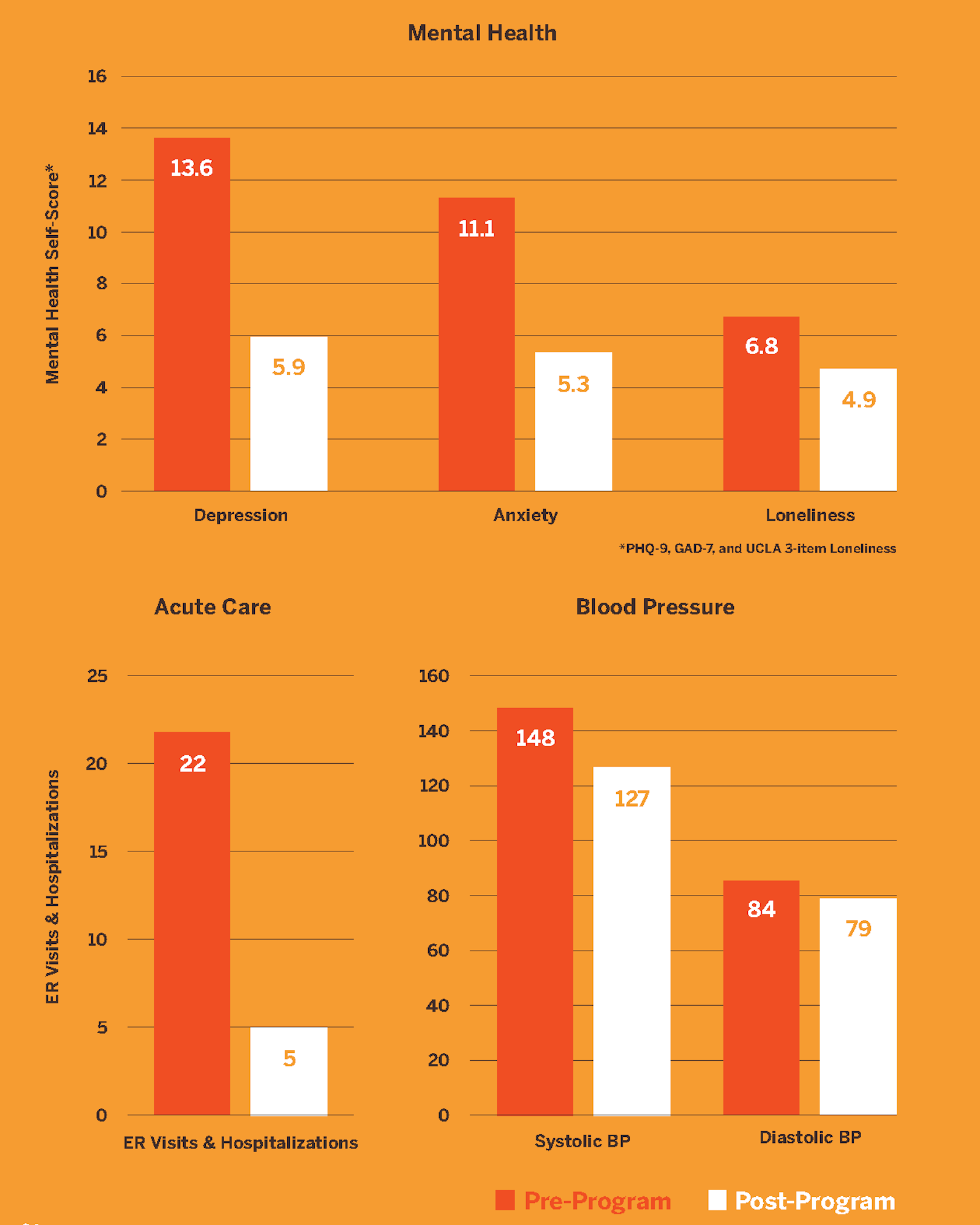
OSW uses industry standard measures to track a range of outcomes including depression (PHQ-9), anxiety (GAD-7), exercise, diet, and blood pressure. Outcomes include reductions in depression, anxiety, social isolation, and loneliness, increases in physical activity and fruit/vegetable consumption, and a 77 percent reduction in Emergency Department visits and hospitalizations. Clearly, these significant outcomes can radically transform the current health and wellness of our country, if a model like ours can be accepted and adopted.
The implications of these outcomes, if taken to scale, are staggering. What if small-group support, health coaching, and experiential medicine formed the foundation of a national clinic-community care strategy?
Revenue Models
Key to our commitment to transforming the standard of clinical care is affordability and revenue/reimbursement structures that make OSW accessible without ongoing grant or philanthropic funding. OSW partners with health insurers, healthcare provider organizations, Federally Qualified Health Centers, low-income housing providers, employers, governments, and other entities to support both patients and staff, and a variety of funding streams are utilized.
One key to sustainability in our partnerships with healthcare delivery systems (clinics and hospitals) is delivering the OSW model as a Group Medical Visit in partnership with clinical providers. OSW contracts with clinics and healthcare delivery systems. The OSW health coaches deliver our signature high-vitality, high-impact weekly program that patients love, while one clinical provider from the clinic conducts short, focused individual visits with each participant, then charts and bills for every patient seen. This enables a clinical provider to see (and bill for) double the number of patients that they would see during the same amount of time in individual visits. The OSW Group Medical Visits (virtual or in-person) generate far more revenue for clinics than they cost to run, and deliver excellent clinical care while improving provider experience. In this way, the OSW model is an example of deep, next-generation clinic-community integration, bringing the community (health coaches, peer leaders) to sustainably animate the clinic as a platform for human thriving.
Clinic Meets Community
Clinical care needs to be one small part of a comprehensive and generative ecosystem of support for well-being. Resilience is a team sport and a resource that is cultivated in relationships! As a field, we need structures that liberate, animate, and activate the power of community, where support and care are mutual and self-sustaining, not extractive. The good news is that humans are hardwired to do this.
This is what we’ve learned at Open Source Wellness. Our work must be generative, both socially and financially, for it to thrive. By utilizing health coaches, peer leaders, and patients’ own experiences and wisdom to foster a culture of care and support, we liberate medical providers to focus on the true medical needs of their patients. Meanwhile, coaches provide the social scaffolding, the “starter culture” that gives rise to the framework, context, and safety for community care to arise naturally.
They key to transforming an exhaustive and extractive clinical system is not more clinical care, or more “self-care.” It’s intentionally-designed social structures that call forth and uplift the resources within and between our patients. It’s bringing clinic and community together, leveraging the synergistic abundance found in partnerships to deliver excellent care, generate revenue, and promote well-being, health, and resilience.
Open Source Wellness cares about health, but beyond that we care about humanity, about creating avenues through which human goodness can flow. James Rouse is famously quoted as saying “A community is a garden in which to grow people.” Open Source Wellness creates communities and cultures in which the natural expression of humanity is health and well-being.
For more information on our work click here.
Curious about implementing Open Source Wellness? Connect with Liz
From Design Museum Magazine Issue 017
Experience Open Source Wellness
How are you doing with each of the four aspects of the Universal Prescription? Try rating each one on a scale from 1-10, with 1 being “I’m nowhere near meeting my goals for this,” and 10 being, “I’m feeling great about this, and my behavior is totally aligned with my values.”

Which ones do you already incorporate effortlessly? Which ones might need a bit more attention, more practice, more cultivation? Then, pick one to focus on first: how might you structure it into your days?
